Val Issa knows three people who have been locally infected with the monkeypox virus.
“I have some friends in Melbourne who have contracted it. They are doing well now. It was terrible for all of them.”
The pain scale for them was “nine to 10 out of 10”.
“I changed my behaviour, I haven’t had sex in quite a while,” the 32-year-old digital marketer for a health company told The Sunday Age, adding he was now more likely to stay home and watch Netflix rather than head out to parties.
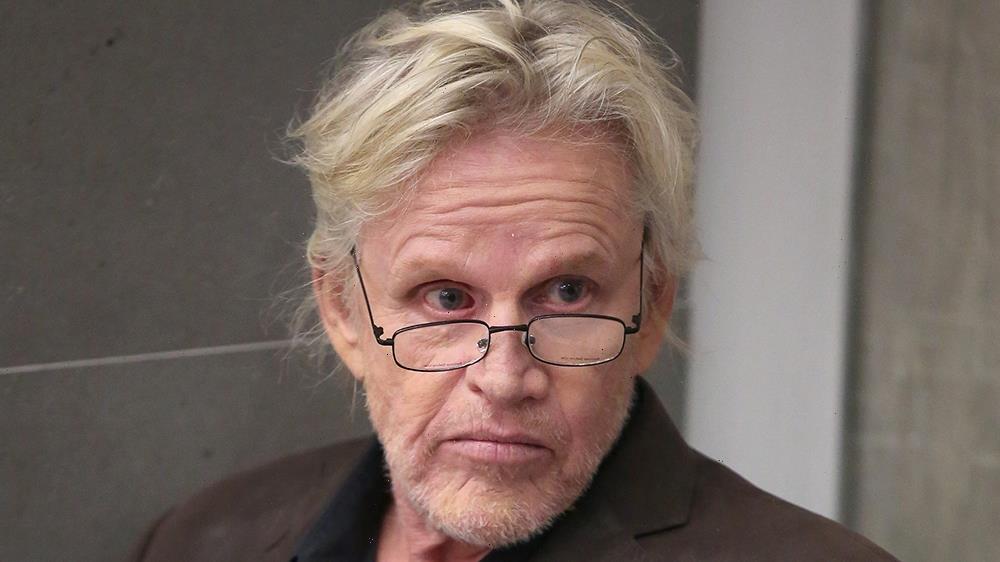
Val Issa has had one dose of the monkeypox vaccine.Credit:Wayne Taylor
“I was being very cautious about not getting close to people.”
He recently went to the gay pub The Peel in Collingwood with a friend visiting from interstate but was cautious about getting close to people.
Issa has managed to have one dose of the 3500 vaccine doses Victoria received earlier this month.
A friend in a high-risk category helped get him an appointment.
“I don’t know anyone else who has got it yet,” Issa said. He has not been able to book a recommended second dose.
Professor Andrew Grulich, head of the HIV epidemiology and prevention program at the Kirby Institute at the University of New South Wales, said the situation was evolving fast.
An image showing oval-shaped monkeypox virions (left) under the microscope.Credit:US Centers for Disease Control
“In Australia we are relying quite a lot on gay community health organisations led by gay men for gay men.
“To talk to people about sex between men can lead to a lot of stigma, but these organisations know how to do it.
“We know from HIV experience that stigma stops people engaging with prevention, it stops them accessing prevention, treatment and care.”
Victoria’s Health Department has said monkeypox may spread through skin-to-skin contact, respiratory droplets or contact with contaminated items or surfaces. Researchers are trying to determine if it can spread via semen.
People who are returning from outbreak hotspots including Europe and North America should monitor for symptoms, it said, and people with monkeypox should isolate and abstain from sex while symptomatic and as a precaution use condoms with sexual partners for eight weeks after infection.
Dave, 50, returned to Melbourne earlier this month from a six-week trip to Europe which cost him thousands of dollars.
Dave, who requested that his real name not be published to protect his confidential medical information, caught monkeypox at an organised sex party in London and made fruitless attempts locally to get treatment before bunkering down at a basic hotel near Heathrow Airport for seven days.
Before he departed, the Melbourne resident tried in vain to get a vaccine at The Alfred hospital and the nearby Prahran Market Clinic. He was knocked back because he was ineligible at the time.
“There was quite strong awareness and a false hope that if people had symptoms, they wouldn’t be attending sex parties,” he said.
“I had organised a pretty special trip to Europe at the cost of thousands of dollars. I knew monkeypox was around, but took a calculated risk as a single gay man.
“Imagine the absolute height of pain of ulcers in your mouth and multiply that by 20.”
“I would certainly hope that anyone who shows any symptoms would pull back from any activity, but we know that not everyone thinks like that.”
The pain was major after his lesions spread inside his mouth and anus. “Imagine the absolute height of pain of ulcers in your mouth and multiply that by 20.”
Grulich said monkeypox could lead to serious illness in some cases. “The worst form of the disease is intra-rectal, which may lead to rectal abscess due to secondary infection. People with severe immune deficiency are more likely to get serious illness due to monkeypox.”
Australia has acquired 450,000 doses of the new third-generation monkeypox vaccine, including 100,000 due to arrive this year and 350,000 next year.
But supplies are currently limited and restricted to people who are having sex with multiple partners, travelling overseas to high-risk areas, or who are immuno-compromised.
“The first consignment of approximately 22,000 have already arrived, with the remaining expected to arrive in the last quarter of 2022 and into 2023,” a federal Department of Health spokeswoman said.
Simon Ruth, chief executive of Thorne Harbour Health, Australia’s oldest LGBTQ health organisation, has criticised the government’s vaccine preparations.
“Montreal had vaccine clinics on the street. They were prepared, Australia was not prepared.”
“The quickest way to get a vaccination is to fly to Montreal,” Ruth said.
At the recent International Aids Conference, held three weeks ago in Canada, all 10,000 delegates were offered the vaccination. Canada approved the vaccine two years ago and stockpiled it.
“Montreal had vaccine clinics on the street,” Ruth said. “They were prepared, Australia was not prepared.
“This could have been foreseeable and other countries did foresee this risk and Australia didn’t.”
Grulich called for more vaccines to be distributed before summer and major LGBTQ events World Pride and Mardi Gras in Sydney next year.
“Here we are doing pretty well but hamstrung by limited vaccine supplies. Before the summer months we really do need to have a well-vaccinated population.
“We need to start vaccinating highly sexually active gay men, but then need to move on to ensure all sexually active gay men can be vaccinated. Before summer would be the timeline.”
The Morning Edition newsletter is our guide to the day’s most important and interesting stories, analysis and insights. Sign up here.
Most Viewed in National
From our partners
Source: Read Full Article