For our free coronavirus pandemic coverage, learn more here.
This week, the Victorian government extended its requirement for vaccination of certain essential workers to all authorised workers in the state. This is a tough call but justified by a unique set of circumstances and the temporary nature of the mandate.
Mandatory vaccination has always been controversial because it comes with significant downsides. There are often better ways to get the high vaccination coverage needed. This new mandate makes access to work and income contingent on receiving this medical intervention for now 1.25 million Victorians.
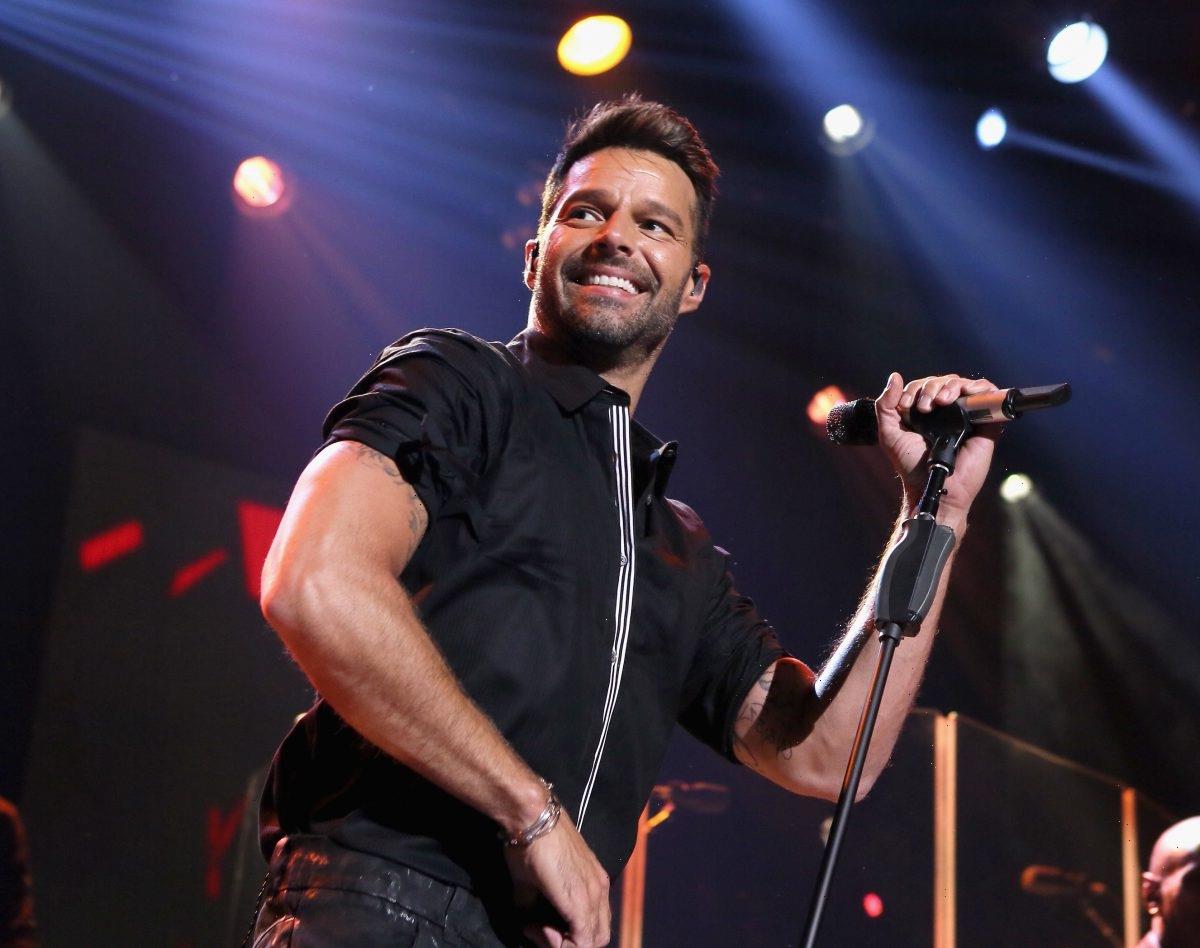
Victorian Premier Daniel Andrews is expanding mandatory vaccinations to cover all authorised workers.Credit:Getty Images
Mandates challenge the foundations of valid consent which says vaccination should be given voluntarily. They can disproportionately affect those lacking access to vaccination or to accurate documentation of the vaccines they have had.
Mandates can lead to conflict between the unvaccinated and those enforcing the requirement and the doctors turning down requests for medical exemptions. And they can reduce trust, particularly among communities affected by past injustices, such as Aboriginal and Torres Strait Islander peoples. Mandates can produce backfire effects among the most vaccine-hesitant for whom autonomy is highly prized, can cause civil unrest and politicisation of vaccination.
This is why mandates for COVID-19 vaccination should only be in place as a last resort and after a government meets a set of prerequisites, outlined in our recent paper.
One of those conditions is a high disease burden. The events of last week put Victoria in this very situation. This was already a delicate time with a rising outbreak against a background of two-dose vaccination coverage at just 52 per cent for those aged 16 years and over – too low to limit the pathway for COVID’s transmission through populations and way below the minimum 80 per cent needed.
Medical staff administer COVID-19 testing in Melbourne. Credit: Getty
But then cases jumped sharply from 990 to 1438 mid-week with more dispersal across regional and rural Victoria – a phenomenon thought to be related to small gatherings across the state for the grand final. This brings the prospect of an outbreak that would see many more hospitalisations and deaths than anticipated in modelling.
Urgently, Victoria needs a precise and effective control strategy and patterns of transmission hold the key. In the NSW outbreak, workplaces have been a main site of transmission where, even amid a lockdown with stringent restrictions, essential workers would still acquire the infection at work, take it home and pass it on to household members, often before realising they had it. Victoria has seen a similar pattern.
For this reason, the government has extended the vaccination requirements to all authorised workers, adding to those already in place for workers in construction, freight, healthcare, aged care and education. Additional workers must have their first vaccine dose by October 15 and their second by November 26.
It is hoped this could stem the flow of transmission and reduce the disease and death otherwise expected.
People check in at a vaccination hub at Whitten Oval on the weekend.Credit:Getty Images
This is a big ask of workers, employers and unions, the latter of whom have largely supported the move. The vaccination services will need to be extremely convenient and able to meet the surge in demand for the unvaccinated workers affected by this strong nudge (or shove). Workers should have paid time off to vaccinate and to manage common side effects, if needed.
A handful – possibly around 5 per cent of workers – may dig in. This is a diverse group, including those who strongly believe the COVID-19 vaccines are unsafe for them to receive, those who are against vaccines in general, those who mistrust medicine and/or government, and those who experience needle phobia.
Employers at the pointy end of mandates enforcing the requirement and those advising non-vaccinators will face correspondence and phone calls from people who are fearful and angry. Often having never discussed vaccination with workers before, they will need strong support.
Under hard mandates, people often try to find workarounds to avoid being vaccinated. One of those is the medical exemption – the only category under which an unvaccinated person can still work. Medical exemptions will apply to only a small group of people. GPs and other doctors asked to sign them may face conflict if the person doesn’t qualify. Their staff may also be affected. These conversations should be supported in a way that is meaningful to those professionals.
GPs and other doctors asked to sign medical exemptions may face conflict if the person doesn’t qualify.
Finally, the affected workers themselves should be supported in considering their options and working out the best path forward. This will often be done in conversations with employers or GPs.
The public health order lifts in mid-December and we are unlikely to see these specific vaccination requirements extended beyond then. Some employees may take leave or resign. This could affect workforce capacity and also needs contingency plans.
Requiring vaccination for work, study, or participation in certain activities must not be done lightly. Mandates should be proportionate, implemented with good process, and as much as possible, consult and help those affected. The gains in population protection must be sufficient to justify the additional coverage needed.
Often a well implemented voluntary program is enough, with access issues addressed and well-placed incentives. Once rapid antigen tests are widely available, it could be sufficient to have mandatory evidence of protection like many countries have implemented in their COVID-19 passports.
Either way, mandates ideally will be a temporary measure until population vaccination is high and where in most settings, risk can be managed. They should be a tool to help us live a COVID-adapted life where the ultimate goal is for us all get back to a more normal life.
Julie Leask is professor at the Susan Wakil school of nursing and midwifery at the University of Sydney. She is an adviser to the World Health Organisation on improving vaccination uptake.
Most Viewed in National
From our partners
Source: Read Full Article