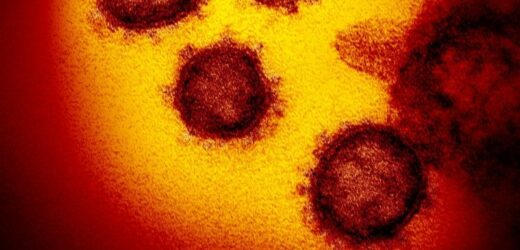
Washington: During those terrifying early days of the pandemic, scientists offered one piece of reassuring news about the novel coronavirus: It mutated slowly. The earliest mutations did not appear to be consequential. A vaccine, if and when it was invented, might not need regular updating over time.
This proved overly optimistic.
The coronavirus, SARS-CoV-2, has had billions of chances to reconfigure itself as it has spread across the planet, and it continues to evolve, generating new variants and subvariants at a clip that has kept scientists on their toes. Two-and-a-half years after it first spilled into humans, the virus has repeatedly changed its structure and chemistry in ways that confound efforts to bring it fully under control.
Despite initial signs that the coronavirus would mutate slowly, it is continuing to “evolve at a fairly rapid rate”. Credit:AP
And it’s not showing signs of settling down into a drowsy old age. Even with all the changes so far, it still has abundant evolutionary space to explore, according to virologists who are tracking it closely. What that means in practical terms is that a virus that’s already extremely contagious could become even more so.
“This virus has probably got tricks we haven’t seen yet,” virologist Robert Garry of Tulane University said. “We know it’s probably not quite as infectious as measles yet, but it’s creeping up there, for sure.”
The latest member of the rogue’s gallery of variants and subvariants is the ungainly named BA.2.12.1, part of the Omicron gang. Preliminary research suggests it is about 25 per cent more transmissible than the BA.2 subvariant that is currently dominant nationally, according to the Centres for Disease Control and Prevention. The CDC said the subvariant has rapidly spread in the north-east in particular, where it accounts for the majority of new infections.
Research assistants analyse the genetic material of COVID-19 caseson sequencing machines in Cambridgeshire, England.Credit:AP
“We have a very, very contagious variant out there. It is going to be hard to ensure that no one gets COVID in America. That’s not even a policy goal,” President Biden’s new COVID-19 co-ordinator, Ashish Jha, said in his inaugural news briefing on Tuesday.
He was answering a question about Vice President Harris, who recently tested positive for the virus and went into isolation. Harris had recently been boosted for the second time – her fourth shot of vaccine.
Her case highlights what has become painfully obvious in recent months: No amount of vaccination or boosting can create a perfect shield against infection from SARS-CoV-2. What the vaccines do very well, however, is greatly reduce the risk of severe illness. That is hugely consequential as a matter of public health, as is the wider use of therapeutics, such as the antiviral Paxlovid.
The vaccines currently deployed were all based on the genomic sequence of the original strain of the virus that spread in late 2019 in Wuhan, China. They essentially mimic the spike protein of that version of the virus and trigger an immune response that is protective when the real virus shows up.
But the variants that have emerged can evade many of the neutralising antibodies that are the immune system’s front line of defence.
“It’s evolving at a fairly rapid rate,” said Jesse Bloom, a computational biologist at the Fred Hutchinson Cancer Research Centre in Seattle. “I do think we need to aggressively consider whether we should update vaccines, and do it soon.”
BA.2.12.1 brings the novel coronavirus up another step on the contagiousness scale. Its close relative, BA.2, was already more transmissible than the first Omicron strain that hit the country in late 2021.
And Omicron was more transmissible than Delta, and Delta was more transmissible than Alpha, and Alpha was more transmissible than earlier variants that did not have the glory of a Greek alphabet name.
Most mutations are not advantageous to the virus. But when a mutation offers some advantage, the process of natural selection will favour it.
There are two fundamental ways that the virus can improve its fitness through mutation. The first could be described as mechanical: It can become innately better at infecting a host. Perhaps it improves its ability to bind to a receptor cell. Or perhaps the mutation allows the virus to replicate in greater numbers once an infection has begun – increasing the viral load in the person and, commensurately, the amount of virus that is shed, potentially infecting other people.
The other strategy involves the workaround of immunity. The human immune system, when primed by vaccines or previous infection to be alert for a specific virus, will deploy antibodies that recognise and neutralise it. But mutations make the virus less familiar to the immune system’s front-line defence.
The subvariants keep coming: Scientists in South Africa have identified BA.4 and BA.5, which have mutations that were seen in earlier variants and could lead to immune evasion.
“The evolution is much more rapid and expansive than we initially estimated,” said Michael T. Osterholm, a University of Minnesota infectious-disease expert. “Every day I wake up, I fear there will be a new subvariant that we will have to consider. . . . We’re seeing subvariants of subvariants.”
Garry, the Tulane scientist, points out that mutations in the virus do not change its appearance dramatically. In fact, he said, even the heavily mutated variants don’t look much different from the original Wuhan strain, or different from other coronaviruses that cause common colds. These are subtle changes.
Garry has a software program that allows him to create a graphic image of the virus, and even rotate it, to observe the locations of mutations and draw inferences for why they matter. On Friday, asked about BA.2.12.1, and why it is spreading, he noted it has a mutation, named S704L, that probably destabilises a portion of the spike protein on the virus’s surface. That essentially loosens up part of the spike in a way that facilitates infection.
This S704L mutation distinguishes this subvariant from BA.2.
The “704″ refers to the 704th position for an amino acid on a chain of roughly 1,100 amino acids that form the protein. The S is one type of amino acid (“serine”) seen in the original strain of the virus, and the L (“leucine”) is what is there after the mutation. (The mutation is caused by a change in one nucleotide, or “letter,” in the genetic code of the virus; three nucleotides encode for an amino acid.)
The virus is spreading today in the United States on an immunological landscape much different from the one it first encountered in early 2020. Between vaccinations and infections, there aren’t many people entirely naive to the virus. The latest CDC data suggest the virus has managed to infect nearly 200 million people in the nation, which has a population of about 330 million. Among children and teenagers, about three out of four have been infected, the CDC estimates.
For the new CDC study, researchers looked at blood samples from thousands of people and searched for an antibody that is found after a natural infection, but not found after vaccination. The CDC concluded that the Omicron variant managed to plow through the United States population during the winter almost as if it were an entirely new virus. The country by then was largely vaccinated. And yet 80 million people, approximately, became infected for the first time in that Omicron wave.
On the family tree of this coronavirus, Omicron is a distant cousin of Delta, Alpha and the other variants that had spread earlier – it came out of virologic left field. No one is sure of the origin of Omicron, but many disease experts assume it came from an immunocompromised patient with a very lengthy illness, and the virus continued to use mutations to evade the immune system’s efforts to clear it.
Omicron was mercifully less likely to kill a person than previous variants. But infectious-disease experts are clear on this point: Future variants could be more pathogenic.
As if mutation wasn’t enough of a problem, the virus has another trick up its sleeve: recombination. It happens when two distinct strains infect a single host simultaneously and their genes becoming entangled. The recombination process is the origin of what’s known as Omicron XE. That recombinant probably emerged from a person co-infected with the original Omicron variant and the BA.2 subvariant.
It was always possible in theory, but the identification of actual recombinants provides “proof of concept,” as Jeremy Luban, a virologist at the University of Massachusetts Medical School, puts it.
The worst-case scenario would be the emergence of a variant or recombinant that renders current vaccines largely ineffective at blocking severe disease. But so far, that hasn’t happened. And no “recombinant” has spread like Omicron or other recent variants and subvariants.
This is the first catastrophic pandemic to occur in the age of modern genomic sequencing. A century ago, no one knew what a coronavirus was, and even a “virus” was a relatively new concept. But today, with millions of samples of the virus analysed at the genetic level, scientists can track mutations virtually in real time and watch the virus evolve. Scientists across the planet have uploaded millions of sequences to the database known as GISAID.
Genomic sequencing has a major limitation in that, although scientists can track changes in the genome, they don’t automatically know what each of those changes is doing to the virus. Which mutations matter most is a question that can be discerned through laboratory experiments, modelling or epidemiological surveillance, but it’s not always simple or obvious.
Erica Saphire, president of the La Jolla Institute for Immunology, speculates that Omicron has mutations that have changed the virus in ways not yet understood but which make it more resistant to antibody-mediated neutralisation.
“It may have acquired some new trick that we haven’t uncovered yet,” Saphire said. “It’s harder to neutralise than I would have expected, based on the number of mutations alone.”
A reality check comes from Jeremy Kamil, associate professor of microbiology and immunology at Louisiana State University Health Shreveport: “These are all SARS-CoV-2.”
What he means is that these are all variations of the same virus, despite what seems like a tremendous amount of mutation. Correspondingly, someone who gets infected with one of these new variants has the same disease as people who got infected previously.
“They got COVID,” he said.
Washington Post
Get a note directly from our foreign correspondents on what’s making headlines around the world. Sign up for the weekly What in the World newsletter here.
Most Viewed in World
From our partners
Source: Read Full Article